Whole-plant cannabis therapy for chronic pain relief
Studies show a variety of individual cannabinoids work against chronic pain—and work even better together
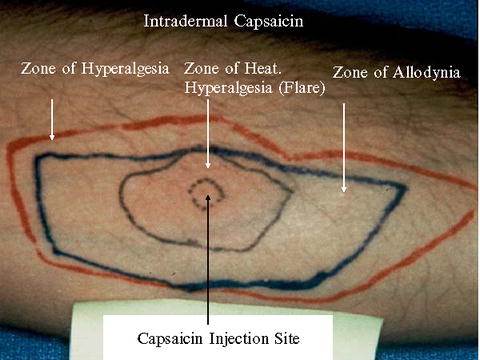
Chronic pain lasts for weeks, months and even years. Often caused by nerve damage (neuropathic pain) or chronic diseases (arthritis, cancer, diabetes, fibromyalgia, multiple sclerosis, etc.), chronic pain can be difficult to treat, frequently requiring treatments just to bring symptoms to a manageable level. Medications include opioid analgesics, anti-inflammatories, anti-epileptics, anti-depressants—and more recently, cannabis.
How cannabis can treat chronic pain
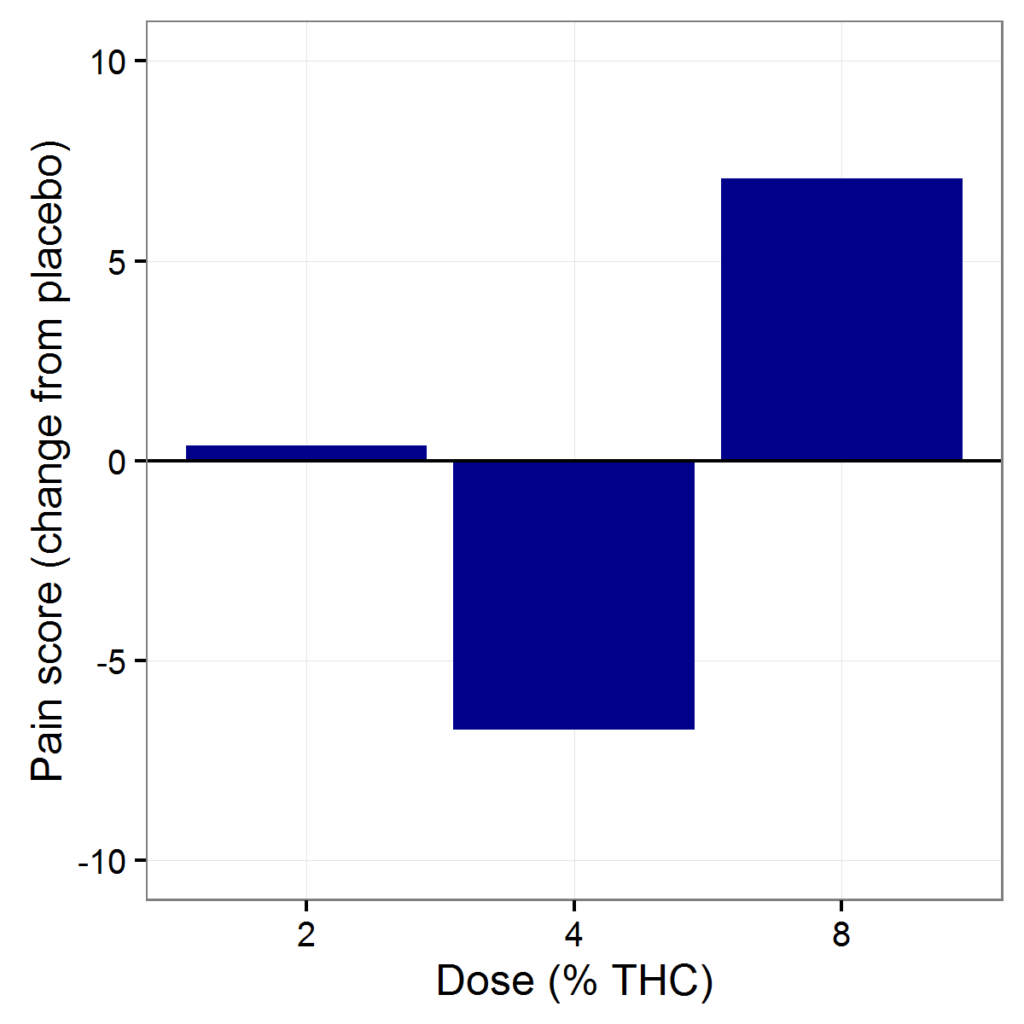
Various studies have examined the analgesic effects of cannabis, often focusing on tetrahydrocannabinol (THC), the cannabinoid, or active ingredient, associated with euphoria. A 2003 study showed that THC enhances the pain-killing effects of opioids, such as morphine.
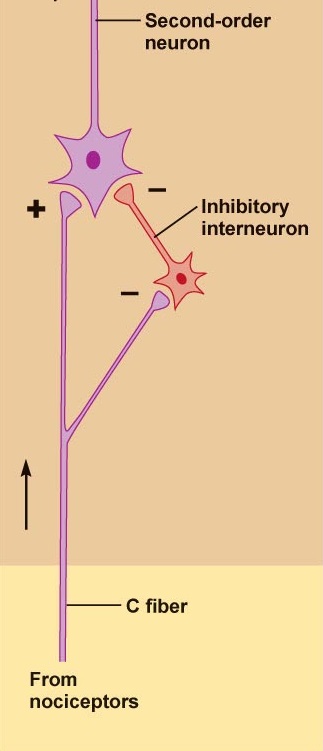
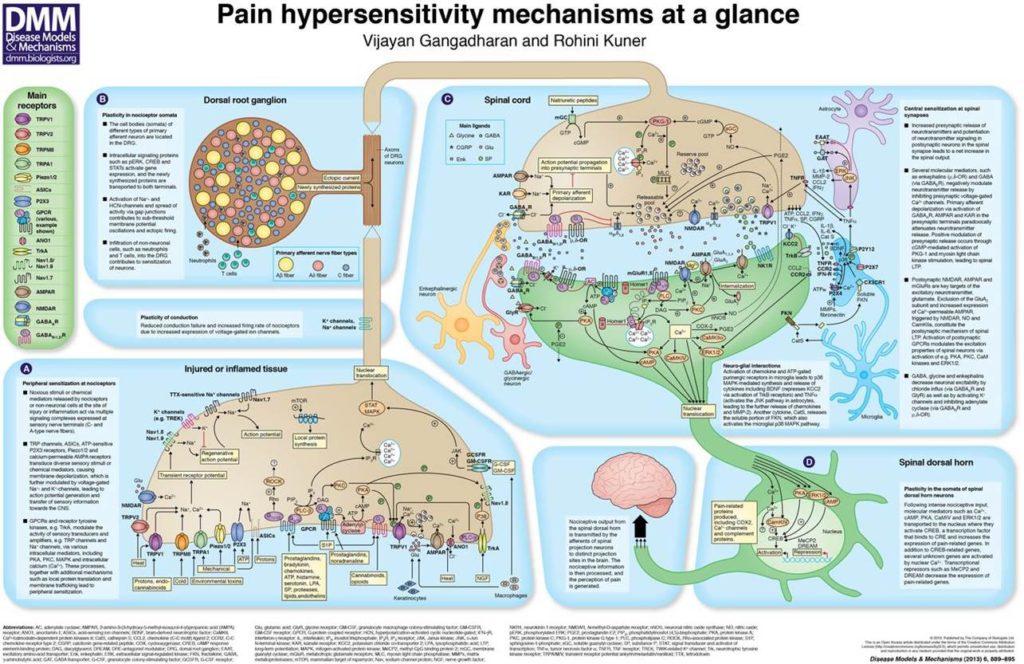
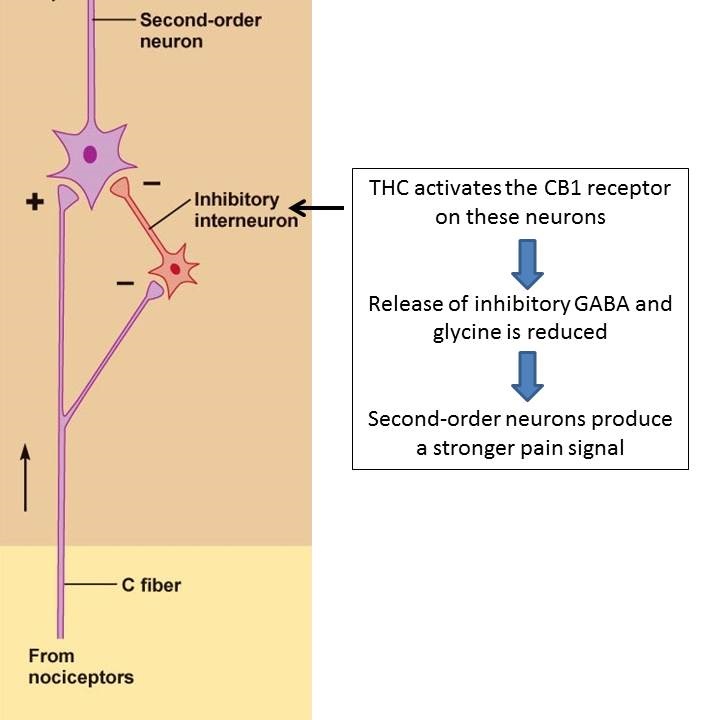
This synergy between opioids and THC is also reflected in chronic pain models, specifically chronic inflammatory and neuropathic pain models. Studies examining THC’s ability to reduce pain show that it works by activating peripheral cannabinoid receptors in the body, namely the CB1 and CB2 receptors.
The role of cannabidiol
Cannabidiol (CBD) has also been examined for its potential as an analgesic, mainly due to growing evidence of its antioxidant, anti-inflammatory, and neuroprotective effects. Research shows that CBD doesn't treat acute pain, but is effective against pathological pain. A 2004 study demonstrated that CBD had potent analgesic effects in inflammatory pain only one hour after single, low dose administration, but no effect on acute internal organ pain.
How CBD works to reduce pain is not clearly known, although some research suggests it may lower levels inflammation-causing cytokines, or cell-signalling molecules. A more recent study suggests CBD may reduce neuropathic pain in rats by targeting amino acid receptors.
More cannabinoids and their effects on the body
Other cannabinoids have shown promise as potential therapeutic treatments for chronic pain. For instance, researchers have found that tetrahydrocannabivarin (THCV) is a CB2 receptor partial agonist—CB2 receptor agonists are effective against many types of pain, including inflammatory, neuropathic, postsurgical and cancer pain. Cannabigerol (CBG) also stimulates cell receptors, demonstrating potential as a pain-reliever in animal models.
What's most effective: extracts or the entire plant?
More research is needed to fully understand cannabis’ potential role in pain management, and to understand the individual impacts of each of its more than 100 different cannabinoids.
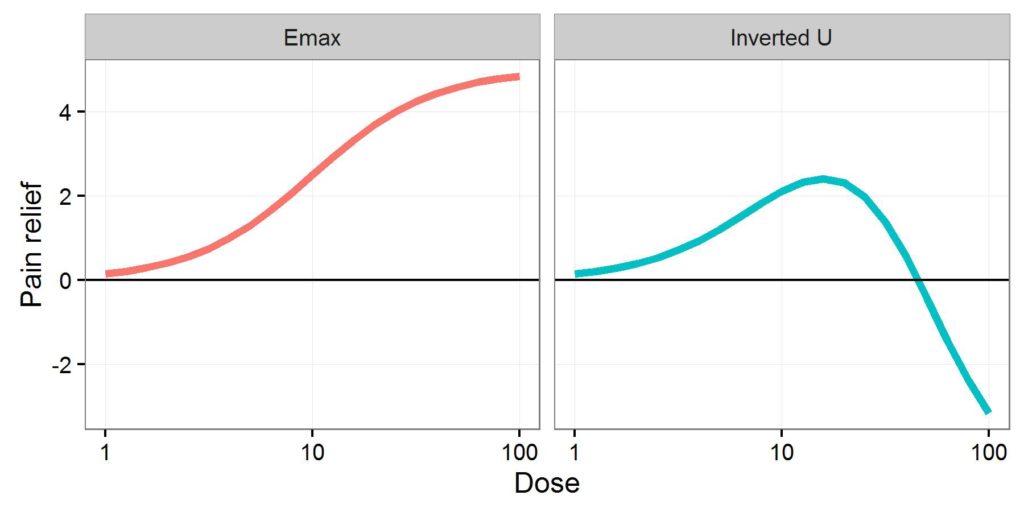
Evidence to support the benefits of whole-plant cannabis extracts instead of single pure cannabinoids is mounting. Studies have shown that extracts produced from the whole cannabis plant are more therapeutic than pure cannabinoid compounds. A 2006 study showed that CBD amplifies the pain-blocking effects of THC.
Another study demonstrated that cannabis extracts containing large amounts of CBD and small amounts of THC, as well as other minor cannabinoids and noncannabinoid components, like flavonoids and terpenes, provided more pain relief than a single pure cannabinoid. In this study, treatment was initially provided with a whole plant extract to gather baseline data. The treatment was then repeated with the same dose, but using only a single pure cannabinoid. The treatment was further repeated using an extract containing both THC and CBD, which also offered less pain relief compared to the whole-plant extract.
All of this suggests the various compounds in the cannabis plant are acting in concert to provide a more profound effect than when taken alone. This effect is referred to as the entourage effect and underscores the importance of the herbal form of cannabis in pain management.
So this goes along with our findings that tinctures that 'steep' for a long period and have whole plant material seem to work better for pain than those that are quick washed.
Studies show a variety of individual cannabinoids work against chronic pain—and work even better together
Chronic pain lasts for weeks, months and even years. Often caused by nerve damage (neuropathic pain) or chronic diseases (arthritis, cancer, diabetes, fibromyalgia, multiple sclerosis, etc.), chronic pain can be difficult to treat, frequently requiring treatments just to bring symptoms to a manageable level. Medications include opioid analgesics, anti-inflammatories, anti-epileptics, anti-depressants—and more recently, cannabis.
How cannabis can treat chronic pain
Various studies have examined the analgesic effects of cannabis, often focusing on tetrahydrocannabinol (THC), the cannabinoid, or active ingredient, associated with euphoria. A 2003 study showed that THC enhances the pain-killing effects of opioids, such as morphine.
This synergy between opioids and THC is also reflected in chronic pain models, specifically chronic inflammatory and neuropathic pain models. Studies examining THC’s ability to reduce pain show that it works by activating peripheral cannabinoid receptors in the body, namely the CB1 and CB2 receptors.
The role of cannabidiol
Cannabidiol (CBD) has also been examined for its potential as an analgesic, mainly due to growing evidence of its antioxidant, anti-inflammatory, and neuroprotective effects. Research shows that CBD doesn't treat acute pain, but is effective against pathological pain. A 2004 study demonstrated that CBD had potent analgesic effects in inflammatory pain only one hour after single, low dose administration, but no effect on acute internal organ pain.
How CBD works to reduce pain is not clearly known, although some research suggests it may lower levels inflammation-causing cytokines, or cell-signalling molecules. A more recent study suggests CBD may reduce neuropathic pain in rats by targeting amino acid receptors.
More cannabinoids and their effects on the body
Other cannabinoids have shown promise as potential therapeutic treatments for chronic pain. For instance, researchers have found that tetrahydrocannabivarin (THCV) is a CB2 receptor partial agonist—CB2 receptor agonists are effective against many types of pain, including inflammatory, neuropathic, postsurgical and cancer pain. Cannabigerol (CBG) also stimulates cell receptors, demonstrating potential as a pain-reliever in animal models.
What's most effective: extracts or the entire plant?
More research is needed to fully understand cannabis’ potential role in pain management, and to understand the individual impacts of each of its more than 100 different cannabinoids.
Evidence to support the benefits of whole-plant cannabis extracts instead of single pure cannabinoids is mounting. Studies have shown that extracts produced from the whole cannabis plant are more therapeutic than pure cannabinoid compounds. A 2006 study showed that CBD amplifies the pain-blocking effects of THC.
Another study demonstrated that cannabis extracts containing large amounts of CBD and small amounts of THC, as well as other minor cannabinoids and noncannabinoid components, like flavonoids and terpenes, provided more pain relief than a single pure cannabinoid. In this study, treatment was initially provided with a whole plant extract to gather baseline data. The treatment was then repeated with the same dose, but using only a single pure cannabinoid. The treatment was further repeated using an extract containing both THC and CBD, which also offered less pain relief compared to the whole-plant extract.
All of this suggests the various compounds in the cannabis plant are acting in concert to provide a more profound effect than when taken alone. This effect is referred to as the entourage effect and underscores the importance of the herbal form of cannabis in pain management.
So this goes along with our findings that tinctures that 'steep' for a long period and have whole plant material seem to work better for pain than those that are quick washed.