Chronic Obstructive Pulmonary Disease (COPD) – Medical Marijuana Research Overview
15 February, 2017
The following information is presented for educational purposes only. Medical Marijuana Inc. provides this information to provide an understanding of the potential applications of cannabidiol. Links to third party websites do not constitute an endorsement of these organizations by Medical Marijuana Inc. and none should be inferred.
The third leading cause of death in the United States, COPD is a group of lung diseases that block airflow and make it difficult to breath. Research indicates that cannabis can help patients manage the pulmonary diseases by reducing airway inflammation and causing bronchodilation.
Overview of COPD
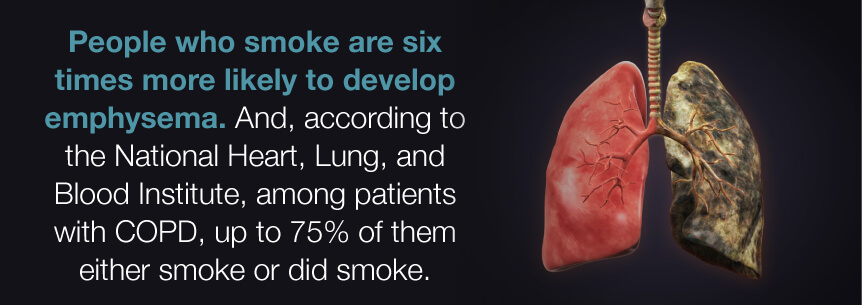
Chronic obstructive pulmonary disease (COPD) is a progressive inflammatory lung disease that obstructs airflow to the lungs and makes it difficult to breathe. In the United States, COPD is most commonly associated with the development of emphysema and chronic bronchitis.
When a person has COPD, less air flows in and out of the airways because either they lose their elastic quality or make more mucus than usual, causing clogging. In chronic bronchitis, the walls of the bronchial tubes become thick and inflamed. In emphysema, the walls between the air sacs can be destroyed, reducing airflow.
COPD is caused by long-term exposure to irritating particulate matter or gases. The number one cause of COPD is cigarette smoking, but other irritants like secondhand smoke, air pollution and workplace exposure to dust and smoke can also pose problems. The disease develops slowly and symptoms get worse over time until even the most basic physical activities, like walking or cooking, became too difficult.
The symptoms associated with COPD typically include the coughing up of large amounts of mucus, shortness of breath, wheezing, and chest tightness. Symptoms often don’t appear until significant damage to the lungs has already occurred. A major cause of disability, COPD is most commonly diagnosed in middle-aged or older adults.
COPD has been shown to increase the risk of respiratory infections, heart problems, lung cancer, high blood pressure and depression.
There is no cure for COPD and as of now, damage to the airways and lungs are irreversible. However, treatments can help control symptoms and reduce the risk of complications and exacerbations. Bronchodilators are medications that can be used to relax the muscles around the airways. Inhaled steroids help reduce airway inflammation.
Findings: Effects of Cannabis on COPD
Studies indicate that cannabis could potentially be therapeutically beneficial for managing acute attacks of airway constriction due to inflammation, thereby acting as a preventative measure for patients with COPD. Cannabis has been shown through numerous studies to have efficacy for reducing inflammation, suggesting it could be effective for helping manage inflamed airways in those with chronic bronchitis5,12,17.
Two of the major cannabinoids found in cannabis, tetrahydrocannabinol (THC) and cannabidiol (CBD) have shown in several studies to have anti-inflammatory benefits through a variety of mechanisms23. THC and CBD interact with the endocannabinoid system’s cannabinoid receptors (CB1 and CB2) to help the body maintain homeostasis. The activation of CB1 and CB2 receptors has shown to reduce airway inflammation4,8. A research review concluded that CBD has a potent anti-inflammatory effect and also improves lung function, suggesting it could be a useful therapeutic tool for the treatment of inflammatory lung diseases16. In an animal study, CBD was shown to have anti-inflammatory effects following acute lung injury9. Studies have also found that terpenes, the aromatic compounds found in cannabis, show anti-inflammatory benefits9.
Some research has also shown that the cannabinoids found in cannabis can have bronchodilatory effects, thereby decreasing resistance in the respiratory airway and increasing airflow to the lungs19. One study found that cannabinoids’ activation of the CB1 receptor inhibits contraction of the smooth muscle surrounding the lungs to dilate the bronchial tubes and further open up the airways9.
It’s important to note that findings in several studies suggest that the smoking of marijuana may increase the prevalence of acute and chronic bronchitis due to irritants entering the lungs20. Heavy smoking of marijuana on its own can cause airway obstruction1,25. These findings suggest that patients with COPD should stick with cannabis products that are delivered through methods other than smoking, such as cannabis oils and edibles.
States That Have Approved Medical Marijuana for COPD
While no states have approved medical marijuana specifically for the treatment of COPD, several states will consider approving medical marijuana for the treatment of other conditions, but require an approval or a recommendation by a physician. These states include: California (any debilitating illness where the medical use of marijuana has been recommended by a physician), Connecticut (other medical conditions may be approved by the Department of Consumer Protection), Massachusetts (other conditions as determined in writing by a qualifying patient’s physician), Nevada (other conditions subject to approval), Oregon (other conditions subject to approval), Rhode Island (other conditions subject to approval), and Washington (any “terminal or debilitating condition”).
In Washington D.C., any condition can be approved for medical marijuana as long as a DC-licensed physician recommends the treatment.
Recent Studies on Cannabis’ Effect on COPD
- CBD has a potent anti-inflammatory effect and also improves lung function, suggesting it could be a useful therapeutic tool for the treatment of inflammatory lung diseases.
Cannabidiol improves lung function and inflammation in mice submitted to LPS-induced acute lung injury.
(http://www.tandfonline.com/doi/full/10.3109/08923973.2014.976794?needAccess=true)
- Cannabis has shown to be effective for treating inflammation.
Cannabinoids, endocannabinoids, and related analogs in inflammation.
(http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2664885/)
- Aldington, S., Williams, M., Nowitz, M., Weatherall, M., Pritchard, A., McNaughton, A., Robinson, G., and Beasley, R. (2007). Effects of cannabis on pulmonary structure, function and symptoms. Thorax, 62(12), 1058–1063. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2094297/.
- Belvisi, M.G. (2008). Preclinical assessment of novel therapeutics on the cough reflex: cannabinoid agonists as potential antitussives. Lung, 186, Suppl 1, S66-9. Retrieved from http://link.springer.com/article/10.1007/s00408-007-9028-8.
- Bento, A. F., Marcon, R., Dutra, R. C., Claudino, R. F., Cola, M., Pereira Leite, D. F., and Calixto, J. B. (2011). β-Caryophyllene Inhibits Dextran Sulfate Sodium-Induced Colitis in Mice through CB2 Receptor Activation and PPARγ Pathway. The American Journal of Pathology, 178(3), 1153–1166. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3070571/.
- Braun, A., Engel, T., Aguilar-Pimentel, J.A., Zimmer, A., Jakob, T., Behrendt, H, and Mempel, M. (2011, April). Beneficial effects of cannabinoids (CB) in a murine model of allergen-induced airway inflammation: role of CB1/CB2 receptors. Immunobiology, 216(4), 466-76. Retrieved from http://www.sciencedirect.com/science/article/pii/S0171298510001592.
- Burstein, S. H., and Zurier, R. B. (2009). Cannabinoids, Endocannabinoids, and Related Analogs in Inflammation. The AAPS Journal, 11(1), 109. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2664885/.
- COPD. (2016, July 12). Mayo Clinic. Retrieved from http://www.mayoclinic.org/diseases-conditions/copd/home/ovc-20204882.
- Costola-de-Souza, C., Ribeiro, A., Ferraz-de-Paula, V., Calefi, A.S., Aloia, T.P.A., Gimenes-Júnior, J.A., de Almedia, V.I., Pinheiro, M.L., and Palermo-Neto, J. (2013). Monoacylglycerol Lipase (MAGL) Inhibition Attenuates Acute Lung Injury in Mice. PLoS ONE, 8(10), e77706. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3808422/.
- Ferrini, M.E., Hong, S., Stierle, A., Stierle, D., Stella, N., Roberts, K., and Jaffar, Z. (2016, December 19). CB2 receptors regulate natural killer cells that limit allergic airway inflammation in a murine model of asthma. Allergy, doi: 10.1111/all.13107. [Epuc ahead of print]. Retrieved from http://onlinelibrary.wiley.com/wol1/doi/10.1111/all.13107/full.
- Grassin-Delyle, S., Naline, E., Buenestado, A., Faisy, C., Alvarez, J.C., Salvator, H., Abrial, C., Advenier, C., Zemoura, L., Devillier, P. (2014). Cannabinoids inhibit cholinergic contraction in human airways through prejunctional CB1 receptors. British Journal of Pharmacology, 171(11), 2767–2777. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4243853/.
- Hartley, J.P.R., Nogrady, S.G., and Graham, J.D.P. (1978). Brochodiltor Effect of Δ1-Tetrahydrocannabinol. British Journal of Clinical Pharmacology, 5, 523-535. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1429361/pdf/brjclinpharm00292-0050.pdf.
- Kemper, J.A., Honig, E.G., and Martin, G.S. (2015, February). The effects of marijuana exposure on expiratory airflow. A study of adults who participated in the U.S. National Health and Nutrition Examination Study. Annals of American Thoracic Society, 12(2), 135-41. Retrieved from http://www.atsjournals.org/doi/full/10.1513/AnnalsATS.201407-333OC.
- Kozela, E., Pietr, M., Juknat, A., Rimmerman, N., Levy, R., and Vogel, Z. (2010). Cannabinoids Δ9-Tetrahydrocannabinol and Cannabidiol Differentially Inhibit the Lipopolysaccharide-activated NF-κB and Interferon-β/STAT Proinflammatory Pathways in BV-2 Microglial Cells. The Journal of Biological Chemistry, 285(3), 1616–1626. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2804319/.
- Patel, H.J., Birrell, M.A., Crispino, N., Hele, D.J., Venkatesan, P., Barnes, P.J., Yacoub, M., and Belvisi, M.G. (2003). Inhibition of guinea-pig and human sensory nerve activity and the cough reflex in guinea-pigs by cannabinoid (CB2) receptor activation. British Journal of Pharmacology, 140(2), 261–268. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1574031/.
- Pickering, E.E., Semple, S.J., Nazir, M.S., Murphy, K., Snow, T.M., Cummin, A.R., Moosavi, S.H., Guz, A., and Holdcroft, A. (2011). Cannabinoid effects on ventilation and breathlessness: a pilot study of efficacy and safety. Chronic Respiratory Disease, 8(2), 109-18. Retrieved from http://journals.sagepub.com/doi/pdf/10.1177/1479972310391283.
- Ribeiro, A., Ferraz-de-Paula, V., Pinheiro, M.L., Vitoretti, L.B., Mariano-Souza, D.P, Quinteiro-Filho, W.M., Akamine, A.T., Almeida, V.I., Quevedo, J., Dal-Pizzol, F., Hallak, J.E., Zuardi, A.W., Crippa, J.A., and Palermo-Neto, J. (2012, March). Cannabidiol, a non-psychotropic plant-derived cannabinoid, decreases inflammation in a murine model of acute lung injury: role for the adenosine A(2A) receptor. European Journal of Pharmacology, 678(1-3), 78-85. Retrieved from http://www.sciencedirect.com/science/article/pii/S0014299912000052.
- Ribeiro, A., Almeida, V.I., Costola-de-Souza, C., Ferraz-de-Paula, V., Pinheiro, M.L., Vitoretti, L.B., Gimenes-Junior, J.A., Akamine, A.T., Crippa, J.A., Tavare-de-Lima, W., and Palermo-Neto, J. (2015, February). Cannabidiol improves lung function and inflammation in mice submitted to LPS-induced acute lung injury. Immunopharmacology and Immunotoxicology, 37(1), 35-41. Retrieved from http://www.tandfonline.com/doi/full/10.3109/08923973.2014.976794?needAccess=true.
- Staiano, R.I., Loffredo, S., Borriello, F., Iannotti, F.A., Piscitelli, F., Orlando, P., Secondo, A., Granata, F., Lepore, M.T., Fiorelli, A., Varricchi, G., Santini, M., Triggiani, M., Di Marzo, V., and Marone, G. (2016, April). Human lung-resident macrophages express CB1 and CB2 receptors whose activation inhibits the release of angiogenic and lymphangiogenic factors. Journal of Leukocyte Biology, 99(4), 531-40. Retrieved from http://www.jleukbio.org/content/99/4/531.long.
- Tan, W.C., Lo, C., Jong, A., Xing, L., FitzGerald, M.J., Vollmer, W.M., Buist, S.A., and Sin, D.D., for the Vancouver Burden of Obstructive Lung Disease (BOLD) Research Group. (2009). Marijuana and chronic obstructive lung disease: a population-based study. CMAJ : Canadian Medical Association Journal, 180(8), 814–820. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2665947/.
- Tashkin, D.P., Shapiro, B.J., and Frank, I.M. (1974, April). Acute effects of smoked marijuana and oral delta9-tetrahydrocannabinol on specific airway conductance in asthmatic subjects. The American Review of Respiratory Disease, 109(4), 420-8. Retrieved from http://www.atsjournals.org/doi/pdf/10.1164/arrd.1974.109.4.420.
- Tashkin, D.P., Baldwin, G.C., Sarafian, T., Dubinett, S., and Roth, M.D. (2002, November). Respiratory and immunologic consequences of marijuana smoking. Journal of Clinical Pharmacology, 42 (11 Suppl), 71S-81S. Retrieved from http://onlinelibrary.wiley.com/doi/10.1002/j.1552-4604.2002.tb06006.x/abstract.
- Tashkin, D.P. (2009). Does smoking marijuana increase the risk of chronic obstructive pulmonary disease? CMAJ : Canadian Medical Association Journal, 180(8), 797–798. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2665954/.
- Tashkin, D.P. (2013, June). Effects of marijuana smoking on the lung. Annals of American Thoracic Society, 10(3), 239-47. Retrieved from http://www.atsjournals.org/doi/full/10.1513/AnnalsATS.201212-127FR.
- Turcotte, C., Blanchet, M.R., Laviolette, M., and Flamand, N. (2016, September 15). Impact of cannabis, cannabinoids, and endocannabinoids in the lungs. Frontiers in Pharmacology, 7, 317. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5023687/.
- What is COPD? (2014, May 22). National Heart, Lung, and Blood Institute. Retrieved from https://www.nhlbi.nih.gov/health/health-topics/topics/copd.
- Yayan, J., and Rasche, K. (2016). Damaging Effects of Cannabis Use on the Lungs. Advances in Experimental Medicine and Biology, 952, 31-34. Retrieved from http://link.springer.com/chapter/10.1007/5584_2016_71.