Cannabis Treatments for Osteoarthritis

(Source)
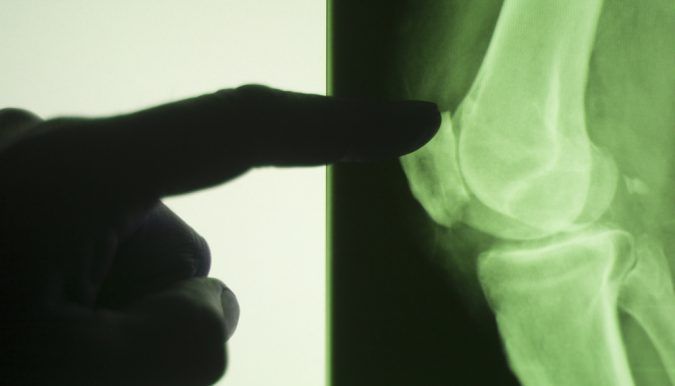
Cannabis is useful for treating a wide range of diseases, including osteoarthritis. According to the Center for Disease Control and Prevention (CDC), one in five non-institutionalized adults with a physical disability are diagnosed with osteoarthritis. It is the most common form of arthritis, and occurs when the protective layer of cartilage around the bones wears down in the joints; the body part affected most often is the knee.
Mainstream treatments for the crippling condition include anti-inflammatory medication, antibiotics, physical therapy, and controversial prescription painkillers. Such options usually come with unwanted side effects that can leave some patients sedated, depressed, or addicted. But now, scientists have found medical marijuana to be beneficial in the fight against osteoarthritis and other forms of the disease.
Going Beyond Chronic Pain

(Source)
There is no doubt that cannabis can be used to address the chronic pain that many patients experience when dealing with the condition. An assortment of organic topical rubs, edibles, and traditional bong rips are effective against extreme pain.
Going beyond this symptom, however, the plant may also be helpful in promoting the functionality of inflamed joints. A study conducted by the University of Nottingham UK, in collaboration with the University of Pittsburgh and Virginia Commonwealth University, suggests that specific cannabinoids are efficient in slowing down the progression of the disease. In particular, the receptor that scientists were working with during the trial was cannabinoid type 2 (CB2).
“Results showed treating osteoarthritis by increasing CB2 receptors with the use of JWH-133 injections reduced chemicals responsible for causing inflammation in osteoarthritis, reduced excitatory nerves in the spine that are stimulated by inflammation, and increased the overall amount of CB2 receptor [message] (MRNA) and protein in nerve cells of the spine,” said Shelley White from Collective Evolution.
In another study pioneered by Dr. Jason McDougall from Halifax University (with a three-year grant from the Arthritis Society), researchers discovered that cannabis may help repair damaged joints affected by the disease. During the trial, scientists also focused on the medicinal properties of non-psychoactive cannabinoids. The group uncovered that marijuana molecules cling to receptors in aching joints and control various neurotransmission signals in the surrounding area.
Obstacles in Treatment

(Source)
Despite being supported by clinical trials and studies, acquiring medical marijuana to treat osteoarthritis might be difficult, depending on where you live in the US. It is important to consider that no states have approved medical cannabis treatments for the illness yet. Some states, like California and New Mexico, allow organic remedies for other types of arthritis. A handful of states, including Connecticut, Massachusetts, Nevada, Oregon, Rhode Island and Washington, acknowledge the use of the plant for osteoarthritis, but a recommendation from a registered physician is required.
Nonetheless, it is possible to use medical marijuana to ease the secondary symptoms associated with the disorder. Patients suffering from chronic pain or “intractable pain” may easily gain access to cannabis treatments, since most states with legal marijuana laws support its use for such conditions.

(Source)
Cannabis is useful for treating a wide range of diseases, including osteoarthritis. According to the Center for Disease Control and Prevention (CDC), one in five non-institutionalized adults with a physical disability are diagnosed with osteoarthritis. It is the most common form of arthritis, and occurs when the protective layer of cartilage around the bones wears down in the joints; the body part affected most often is the knee.
Mainstream treatments for the crippling condition include anti-inflammatory medication, antibiotics, physical therapy, and controversial prescription painkillers. Such options usually come with unwanted side effects that can leave some patients sedated, depressed, or addicted. But now, scientists have found medical marijuana to be beneficial in the fight against osteoarthritis and other forms of the disease.
Going Beyond Chronic Pain

(Source)
There is no doubt that cannabis can be used to address the chronic pain that many patients experience when dealing with the condition. An assortment of organic topical rubs, edibles, and traditional bong rips are effective against extreme pain.
Going beyond this symptom, however, the plant may also be helpful in promoting the functionality of inflamed joints. A study conducted by the University of Nottingham UK, in collaboration with the University of Pittsburgh and Virginia Commonwealth University, suggests that specific cannabinoids are efficient in slowing down the progression of the disease. In particular, the receptor that scientists were working with during the trial was cannabinoid type 2 (CB2).
“Results showed treating osteoarthritis by increasing CB2 receptors with the use of JWH-133 injections reduced chemicals responsible for causing inflammation in osteoarthritis, reduced excitatory nerves in the spine that are stimulated by inflammation, and increased the overall amount of CB2 receptor [message] (MRNA) and protein in nerve cells of the spine,” said Shelley White from Collective Evolution.
In another study pioneered by Dr. Jason McDougall from Halifax University (with a three-year grant from the Arthritis Society), researchers discovered that cannabis may help repair damaged joints affected by the disease. During the trial, scientists also focused on the medicinal properties of non-psychoactive cannabinoids. The group uncovered that marijuana molecules cling to receptors in aching joints and control various neurotransmission signals in the surrounding area.
Obstacles in Treatment

(Source)
Despite being supported by clinical trials and studies, acquiring medical marijuana to treat osteoarthritis might be difficult, depending on where you live in the US. It is important to consider that no states have approved medical cannabis treatments for the illness yet. Some states, like California and New Mexico, allow organic remedies for other types of arthritis. A handful of states, including Connecticut, Massachusetts, Nevada, Oregon, Rhode Island and Washington, acknowledge the use of the plant for osteoarthritis, but a recommendation from a registered physician is required.
Nonetheless, it is possible to use medical marijuana to ease the secondary symptoms associated with the disorder. Patients suffering from chronic pain or “intractable pain” may easily gain access to cannabis treatments, since most states with legal marijuana laws support its use for such conditions.